Danny Katz
Executive Director, CoPIRG
Executive Director, CoPIRG
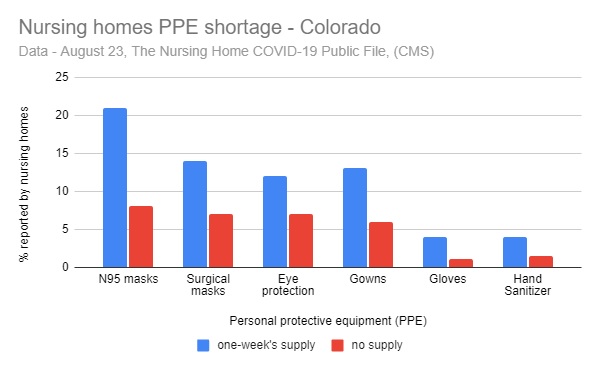
Colorado nursing homes, along with thousands nationwide, are dealing with horrific shortages of masks, gowns and other items they need to protect residents, workers and the broader community from COVID-19. When nursing homes don’t have enough personal protective equipment (PPE), it can lead to outbreaks among residents and staff, worker quarantines and shortages, and more risk to workers’ and residents’ families and neighborhoods.
“It’s maddening that Colorado is dealing with severe PPE shortages at this point in the pandemic, especially in our nursing homes where some of our most vulnerable community members live,” said Danny Katz, Director of CoPIRG. “Without proper PPE nursing home cases can spread rapidly, putting others at risk inside and outside the facility.”
Seven months into this pandemic, PPE shortages nationally have become much worse, according to “Nursing home safety during COVID: PPE shortages,” a report by CoPIRG Foundation and Frontier Group. Our analysis of data submitted to the Centers for Medicare & Medicaid Services by the nation’s 15,000 nursing homes including over 200 in Colorado shows that as of August 23rd:
“Seven months into the pandemic, the number of nursing homes without key supplies has to be zero. We’re failing to protect nursing home residents, we’re failing to protect nursing home workers, and we’re failing to protect all the other Coloradans who they come in contact with. I’m most shocked that the number of nursing homes nationally out of PPE actually tripled between July and August. We can and must do better,” Katz said.
Katz added that experts believe PPE shortages have continued to get worse. One group, GetUsPPE, a grassroots movement founded by medical professionals on the COVID frontlines, said more facilities across all sectors were complaining of shortages in September.
Medical experts believe the shortage of PPE is a key reason that outbreaks and deaths from COVID-19 are disproportionately high in nursing homes.This issue becomes even more urgent with talk of a herd immunity strategy that would allegedly safely cordon off nursing home residents and other at-risk populations while COVID tears through the rest of society. In reality, evidence suggests that until we have a vaccine, without a stronger adherence to spread-prevention practices that usually involve PPE, infection will likely run rampant.
CoPIRG calls for a number of policy actions to improve the supply and transparency of PPE, including:
The PPE shortage is among the problems brought to light by the CMS data on nursing homes. We will explore various issues in a series of reports in the months ahead.
Along with the new report, CoPIRG also released a new guide with COVID-related questions you should ask nursing homes that your loved ones are in or that you are considering and two videos to help people look up PPE supply information for specific nursing homes. All this information can be found at https://copirg.org/feature/usp/nursing-home-safety-during-covid-ppe-shor…